A 50 year old female came to OPD for dialysis.
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians singned informed consent. Here we discuss our individual patients problems with an aim to solve the patient’s clinical problem with collective current best evident based input.
This E blog also reflects my patient cantered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history, clinical findings,investigations and come up with diagnosis and treatment plan.
This is the case of a 50 year old female daily worker by occupation resident of
CHIEF COMPLAINTS: bipedal edema, facial puffiness, darkening of face, severe lower back pain.
HISTORY IF PRESENTING ILLNESS:
Patient was apparently asymptomatic 14 months ago.
She then developed pedal edema, pacial puffiness, sever lower back pain.
She was taken to nalgonda private hospital where they put her medication for 5 days.
The symptoms did not subside so she was brought to Kamineni narketpally.
She undergoes Dialysis for every 4 days since one year.
Past history :
Generalised weakness
Known case of diabetes since 10 years.
Known case of hypertension.
N/K/C/O of asthma, thyroid disorders.
FAMILY HISTORY:
No family history.
PERSONAL HISTORY:
Mixed diet
Loss of appetite
Inadequate sleep
Irregular bowl and bladder movements
No History of alcohol and tobacco addiction
GENERAL EXAMINATION:
Prior consent was taken and patient was examined in a well lit room.
Patient was conscious, coherent and cooperation.
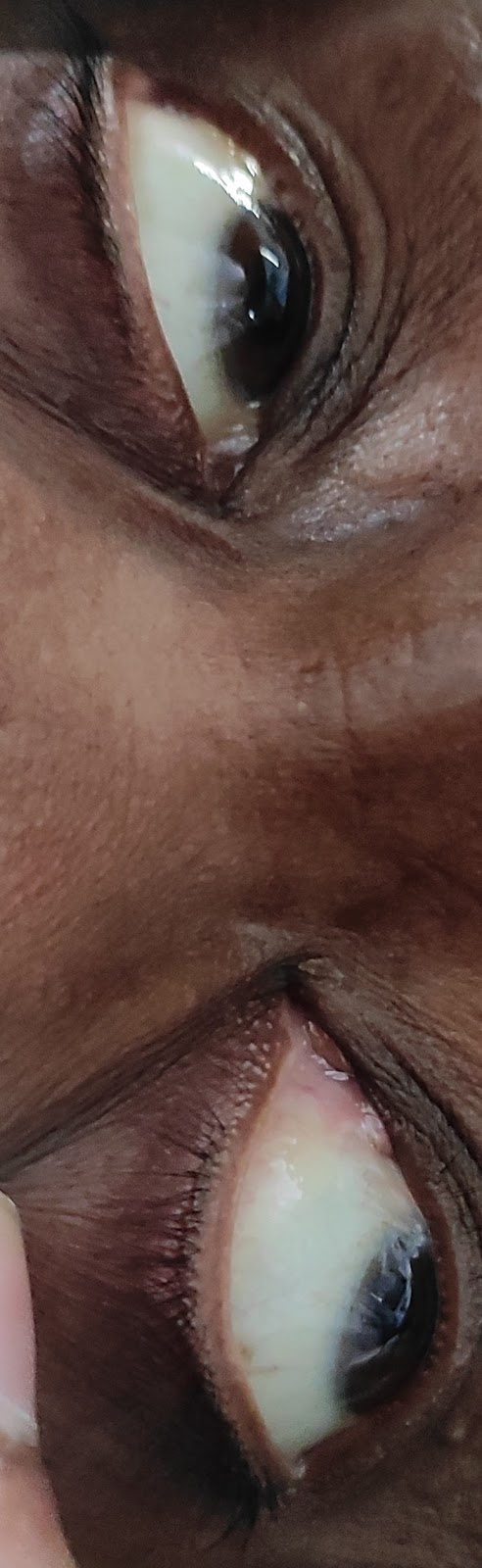
Pallor present . No icterus, clubbing ,cyanosis.
No generalised lymphadenopathy.
Bipedal edema present .
VITALS :
Temperature- 98.7°F
BP-130/90
PR_98 bpm
RR-16 per min
Spo2-98%
GRBS:153%
SYSTEMIC EXAMINATION:
RS: Bilateral chest air entry,
CVS: S1,S2 positive
PA: soft, no tenderness
CNS : Hmf+intact
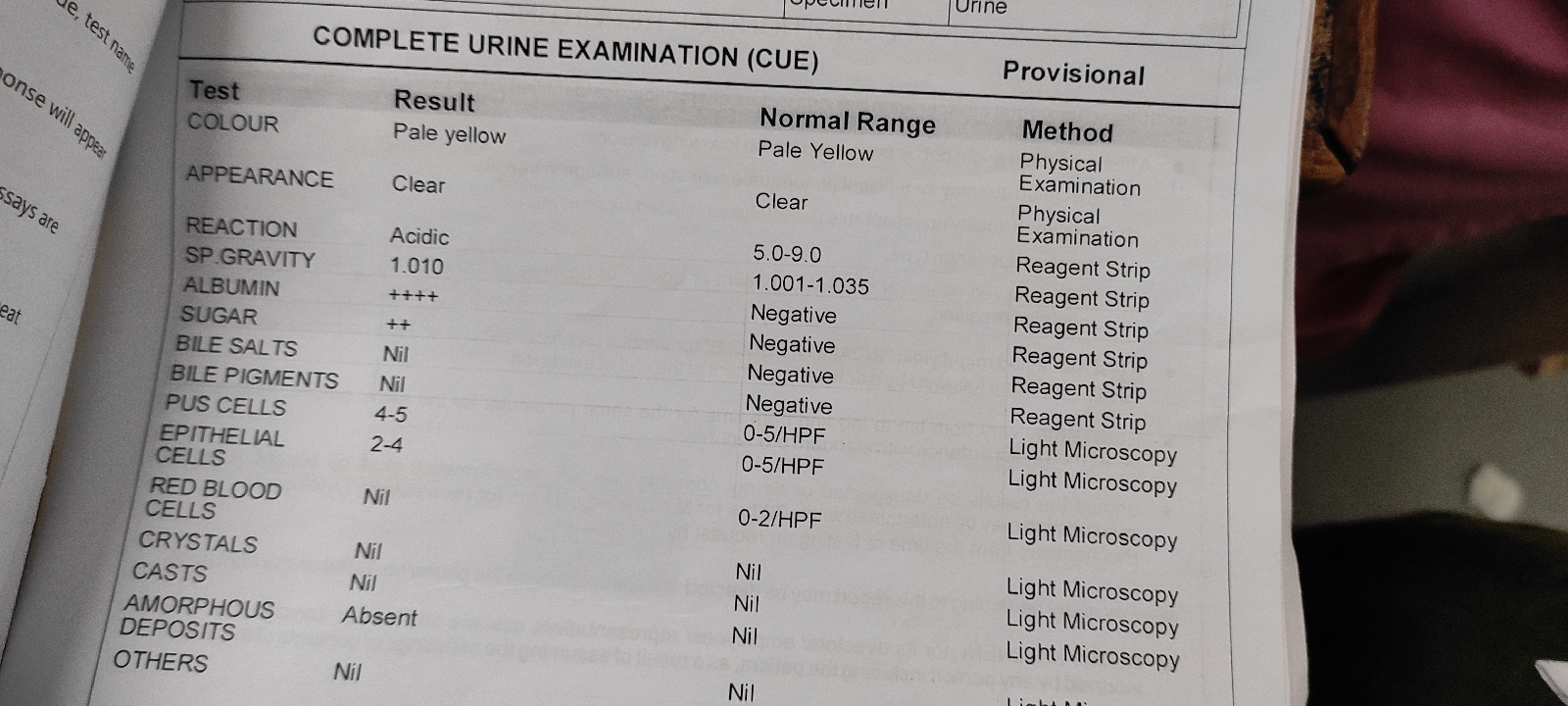
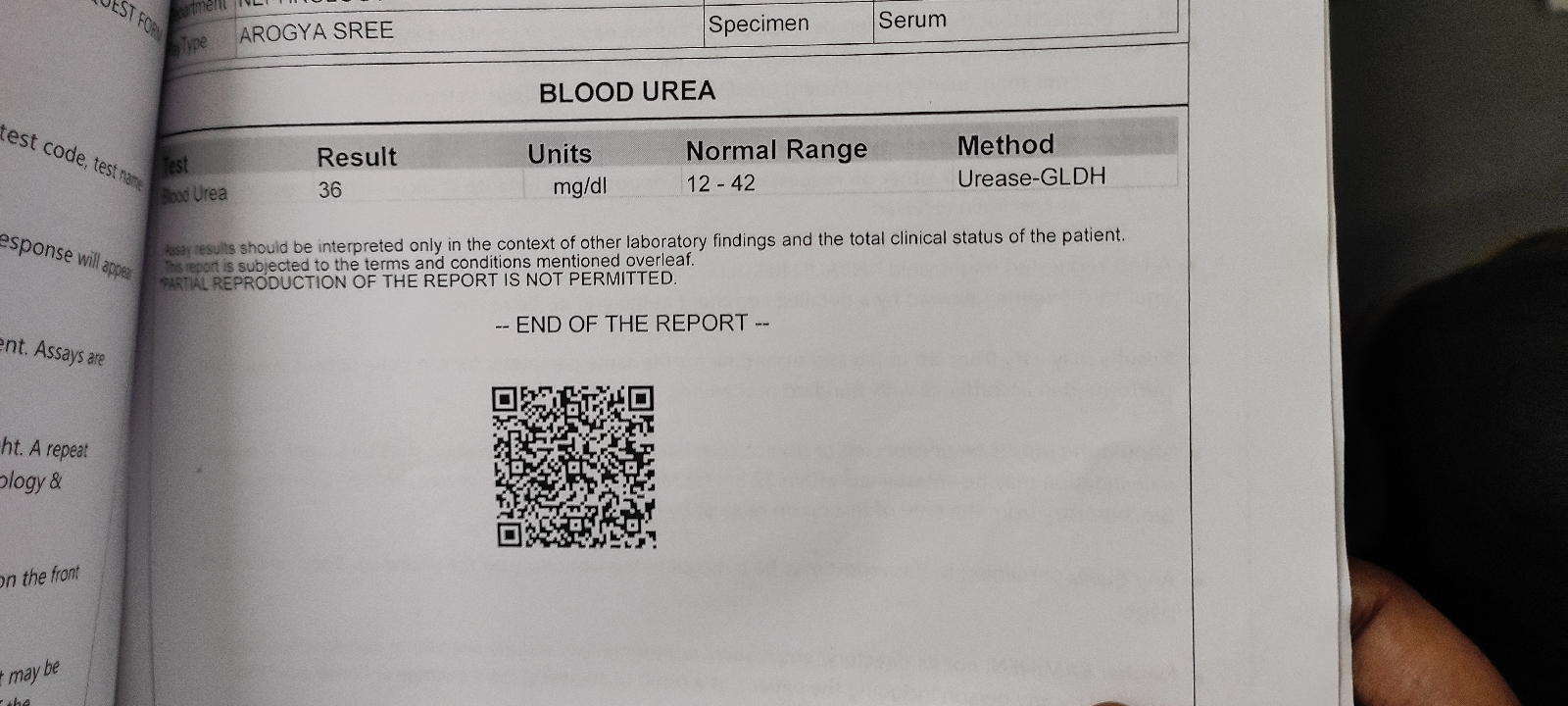
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS :
Renal failure.














Comments
Post a Comment